Faced with indignation from two former prime ministers, several national treasures, an Olympic hero and a leading prostate cancer charity, the head of the UK’s National Screening Committee (NSC) strayed from his evidence-based approach into something more intimate.
“I haven’t previously said this publicly – I have actually had prostate cancer myself,” said Professor Sir Mike Richards, the committee chair. “So I do know what it’s about from a personal angle as well as looking at the evidence.”
The NSC disappointed campaigners by rejecting calls for a national prostate screening programme last week, saying it would do more harm than good for most men.
“It’s not that I’m against having screening,” Richards said, revealing that his prostate had been removed. “Of course I would like to have a screening programme.” But the evidence did not support it, he said.
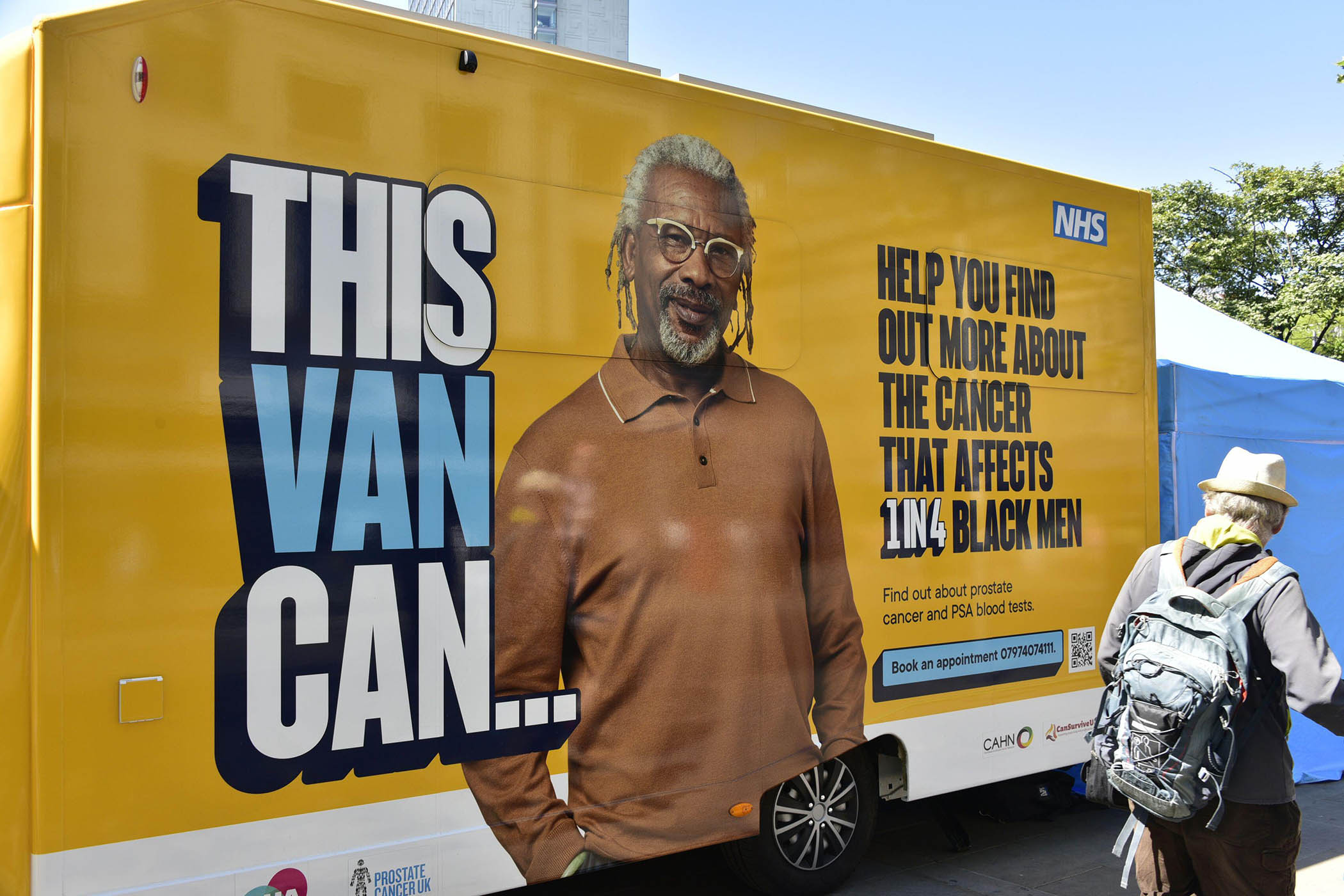
The NSC published draft guidance, advising chief medical officers of the four UK nations that only men with the BRCA1 and BRCA2 genes, who are more at risk, should be screened, in a two-year cycle from the ages of 45 to 61. But it did not support wider screening of black men, because although they are more at risk of getting prostate cancer, there was not evidence that they were more at risk of getting an aggressive, life-threatening form of the disease.
The decision revealed divisions between charities and campaigners, who all agree that action is needed to reduce prostate cancer’s toll on men in the UK, with 55,000 new cases a year and 12,000 deaths.
Those calling for screening now included Sir Chris Hoy, the 49-year-old cyclist who is dying from prostate cancer. He said the NSC decision was “extremely disappointing”, and was joined by Rishi Sunak, David Cameron, actors Sir Stephen Fry and Sir Tony Robinson, the footballer Les Ferdinand and journalist Dermot Murnaghan. “Men will die,” Sunak said. “We are letting down too many men,” Cameron said. Fry said he hoped “the country sees sense”.
Nick Jones, the founder of Soho House, has become a leading campaigner and trustee of Prostate Cancer Research after he was diagnosed in 2022 thanks to a six-monthly private screening programme. He appealed to Wes Streeting, the health secretary, to overrule the committee’s advice, and challenged Richards on Radio 4’s Today programme, when the oncologist revealed he had previously had prostate cancer.
Related articles:
“I think it’s a huge missed opportunity,” said Jones, who is a member of the board of Tortoise Media, which owns The Observer. Richards knew what to do, but many men were not as well informed, Jones said.
Yet while Prostate Cancer Research thinks there is evidence now to support a screening programme, Prostate Cancer UK is backing an ambitious £42m clinical trial, Transform. Last week it began recruiting 16,000 men to compare four methods of screening, and stage two will see 300,000 men test the most promising options.
Newsletters
Choose the newsletters you want to receive
View more
For information about how The Observer protects your data, read our Privacy Policy
At the heart of the issue is the Prostate Specific Antigen (PSA) test, a blood test which detects levels of a protein created by the prostate gland. It is often inaccurate – nearly three-quarters of positive results are for men who are cancer-free, and the test misses about 15% of tumours.
Other tests are on the horizon, but in the meantime, an accurate diagnosis starts with a PSA test, followed by an MRI scan, and finally a biopsy.
Not all prostate cancer cases are the same. Some are aggressive and life-threatening. Yet many are unlikely to grow. A 2008 study looked at three treatment options: active surveillance – regular tests to see if the cancer is progressing; or radiotherapy; or surgery to remove the prostate, and found very little difference in survival rates between them.
But science has moved on, and the NSC asked the Sheffield Centre for Health and Related Research to model the effects of a new screening programme.
It found that of 1,000 men screened, two lives would be saved, but 20 would be diagnosed and 12 would have unnecessary treatment.
That unnecessary treatment usually involves prostate removal – which, in turn, leads to long-term incontinence and impotence.
“It’s about philosophy really, rather than medicine,” said Dr Alastair Lamb of Barts Cancer Institute. “If you had an unlimited supply of healthy uncles, how many of them would you be happy to harm to make a difference to one? Twenty? Ten? Five?”
Photograph by Terry Waller/Alamy Live News